Predictive healthcare taking an ominous turn: a glimpse into the dark side of predictive health systems where algorithms forecast your demise
In a world that feels increasingly reminiscent of a dystopian novel, the concept of a machine predicting one's death is no longer a far-fetched idea. This technological advancement is now a reality in labs and clinics across the globe.
As predictive algorithms become more powerful and prevalent, the need for informed consent evolves. Patients should have the right to opt out of death predictions, ensuring they maintain control over their personal information and destiny. The advent of these algorithms raises old philosophical questions in new digital forms, such as how much we should know about the future and who decides.
The use of these algorithms is transforming medicine, shifting the focus from reaction to prevention. Early warning systems offer both hope and fear. Knowing one's mortality risk could empower individuals to change their habits or seek treatment sooner, but could also lead to anxiety or fatalism.
The "black box" problem exists in many death-predicting algorithms, making it hard to challenge or understand a prediction due to their complexity. Machine learning models learn to predict mortality by analyzing which combinations of factors led to mortality in the past, such as age, blood pressure, cholesterol, family history, and subtle clues hidden in lab results.
For doctors, predictive algorithms are a mixed blessing. They help identify at-risk patients and support difficult decisions, but also cause confusion, second-guessing, and conflict with families. The use of these algorithms in pediatric care raises unique ethical questions, such as whether parents should be told if their child is at high risk.
The risk of false alarms, missed diagnoses, or overconfident prognoses is real due to incomplete or skewed medical records and the potential for algorithms to be fooled by missing data or biased samples. If you knew when your time would come, you might use that knowledge to give your hours more life than simply more hours, focusing on meaning, and finding coherence and healing in storytelling or reflection.
As we hand more of our fate over to machines, our relationship with death itself may change. This transformation could lead to bravery, kindness, and a focus on what matters, or it could haunt us and cast a shadow over every joy.
Predictive healthcare, utilizing artificial intelligence (AI), is becoming increasingly prevalent in hospitals and clinics worldwide. Hospitals worldwide are already using death-predicting algorithms, with some health systems flagging patients at high risk of dying within the next year.
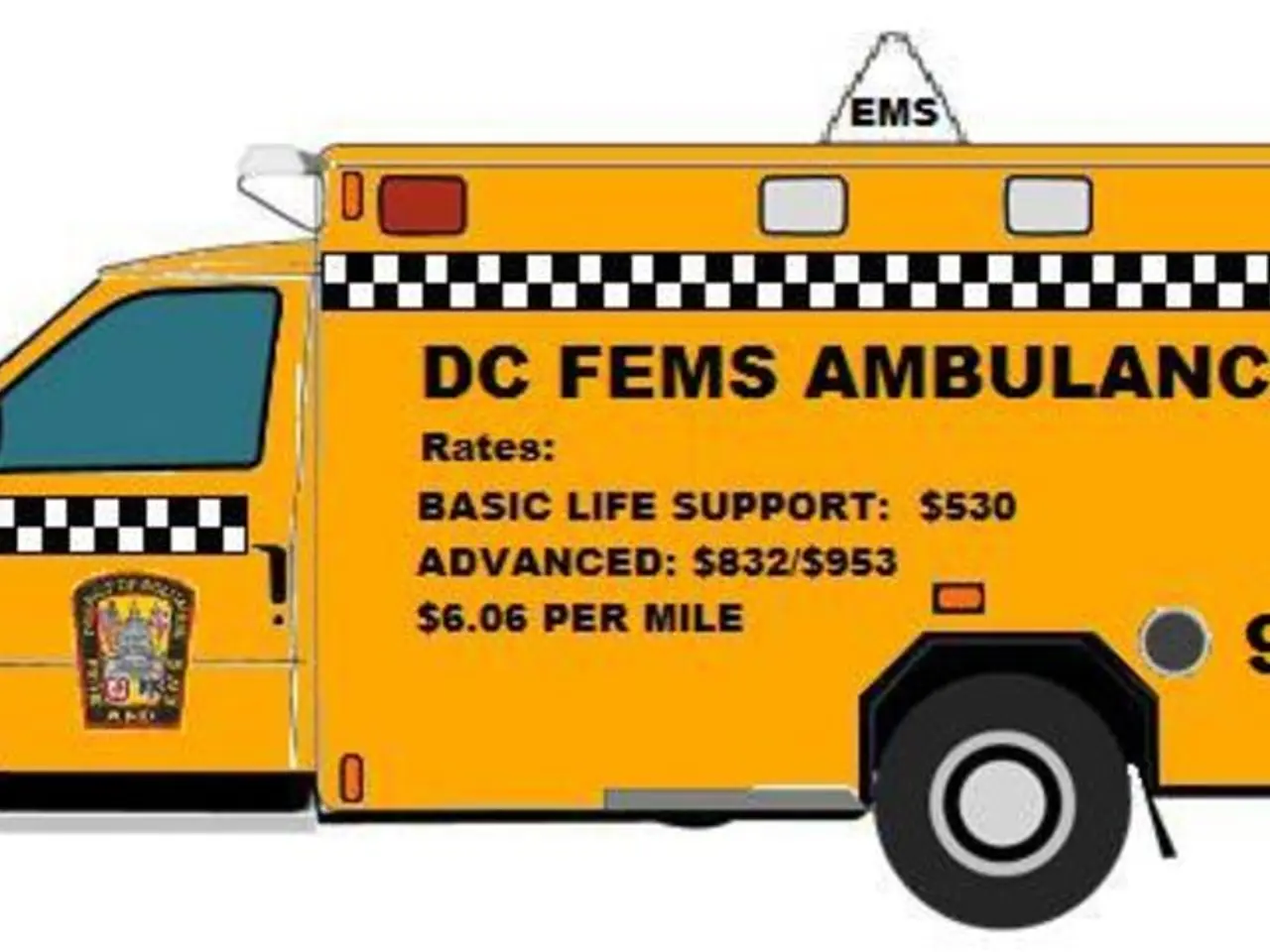
Employers may be tempted to screen candidates based on health risks predicted by AI algorithms, and insurance companies are exploring AI to price policies more accurately or to deny coverage based on predicted health risks. Some AI algorithms go beyond risk scores, generating personalized death timelines that estimate not just if, but when and how a person might die.
AI systems analyze vast amounts of digitized medical data to spot patterns that are difficult for human eyes to discern, helping doctors predict diseases like cancer earlier, suggest personalized treatments, and anticipate complications before symptoms appear.
Responses from individuals when told they have a high chance of dying soon range from panic and denial to relief and resolve. Predictive algorithms hold real promise in identifying risks early, helping people change course, quitting smoking, eating better, or getting screened for disease.
Privacy concerns arise as algorithms crunch through reams of personal data, such as medical records, genetic information, and wearable device data. The ethics of predictive healthcare are complex, raising questions about the right to know one's predicted death date, the potential for discrimination, and the impact on mental health.
As we navigate this new frontier in healthcare, it is crucial to address these ethical dilemmas and ensure that the benefits of predictive algorithms are harnessed responsibly, promoting a future where machines aid us in living longer, healthier, and more fulfilled lives.
Read also:
- Peptide YY (PYY): Exploring its Role in Appetite Suppression, Intestinal Health, and Cognitive Links
- Toddler Health: Rotavirus Signs, Origins, and Potential Complications
- Digestive issues and heart discomfort: Root causes and associated health conditions
- House Infernos: Deadly Hazards Surpassing the Flames